In today's fast-paced world, worry and chronic stress have become everyday experiences for many. Our constant exposure to social media feeds and 24-hour news updates means our brains are flooded with anxiety-provoking content almost nonstop. Even with years of economic expansion, uncertainty around jobs, finances, and the future has only increased. At work, the pressure to multitask and “do more with less” has fragmented our focus and elevated anxiety levels across the board. As these stressors pile up, finding effective, research-based ways to calm the mind has never been more essential.
If you're grappling with ongoing anxiety, chances are that excessive worry plays a major role. While worrying can sometimes feel useful—helping you plan ahead or avoid potential pitfalls—it often backfires. For many people, worry becomes a source of distress rather than a helpful strategy. Fortunately, cognitive behavioral therapy (CBT) offers practical tools to address this cycle. One evidence-based CBT technique involves evaluating whether your worry is productive or unproductive. When a worry is identified as unproductive, it's easier to release it, rather than ruminate endlessly.
To start this process, try asking yourself a few key CBT-inspired questions designed to clarify whether your worry is helping or harming. These self-reflection questions can bring clarity and interrupt the worry loop, allowing you to regain a sense of calm and control.
Cognitive Restructuring: 5 Questions to Get Rid of Intrusive Thoughts and Worry
1. What do you predict will happen, and what is the likelihood it will happen? Identify in detail what you are most concerned will happen. If it’s giving a speech, it may be people laughing at or heckling you. If you’re worried about a difficult interaction with someone, you may fear someone will yell at you or reject you in some way. If the concern is about making a mistake at work, you may fear being fired. Whatever the situation, consider what it really is that you are most afraid of. Oftentimes, just specifically identifying what we fear can help us realize our anxiety may be unfounded.
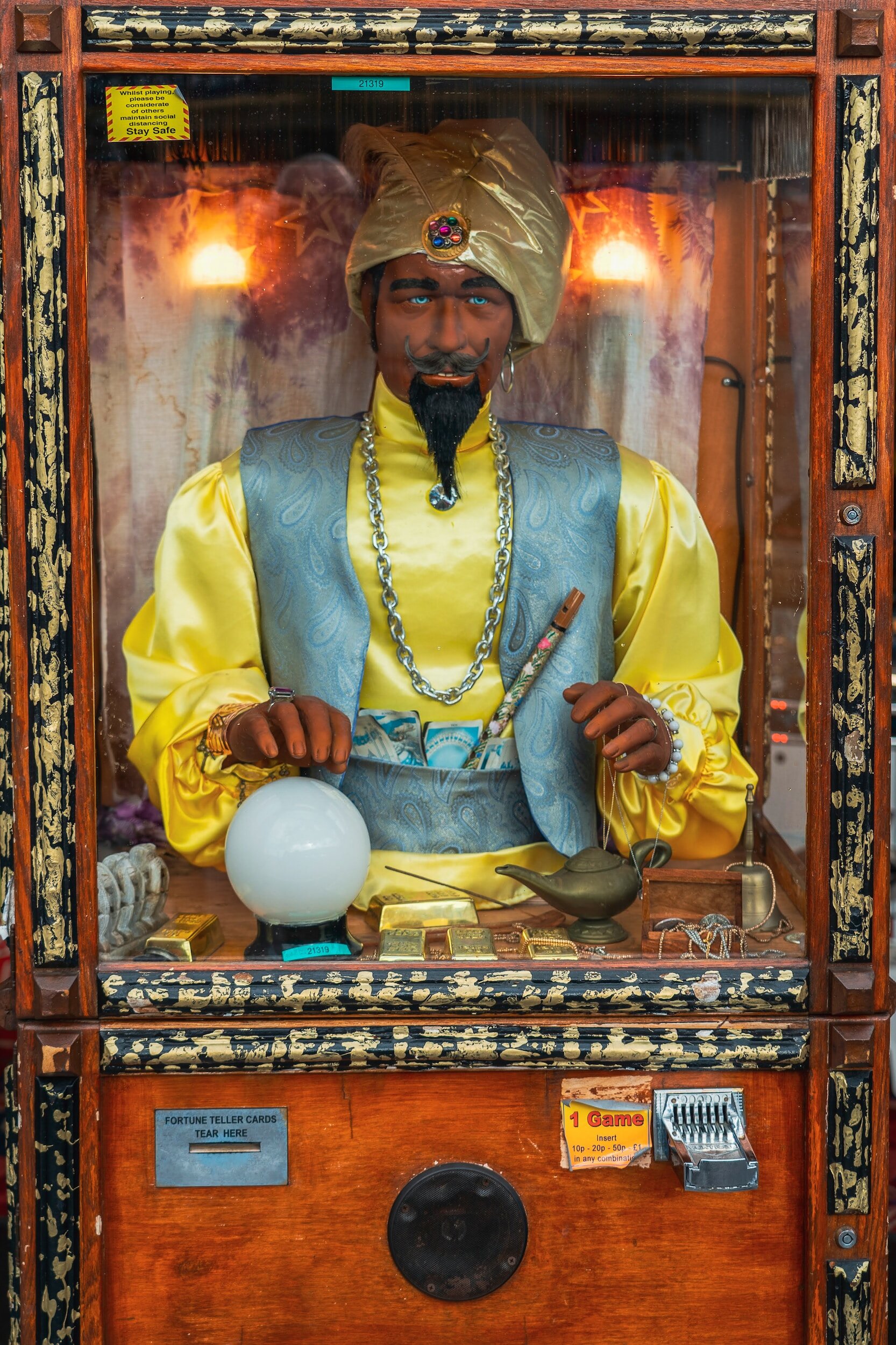
Once you identify the perceived threat, make some evidence-based predictions about how likely the threat is: Is this an accurate prediction, or is this fortune telling? How many times have you experienced this worst-case scenario before? (Does the person you’re thinking about often yell at others? Is it common for you or someone else to be laughed at during speeches? How often are people fired at your work, and when they are, what sorts of/how many infractions lead to their firing?) Would there be steps you could take to reduce the likelihood of your fear coming true? Could you, for instance, craft a sensitive way of being assertive in your feared interaction? How could you influence the outcome more in your favor? Given the situation you fear, is this a plausible outcome? (Do you really think people will heckle you at a professional conference?)
2. What are the best case scenario and most likely scenarios? Some people are already experts at identifying the worst-case scenario. In fact, they’re so good at it that they forget to consider other possibilities. It is helpful also to consider the best-case scenario, which is often equally as plausible as the worst-case. Finally, after identifying the extremes, consider what the most likely scenario is. Usually, our minds drift toward the more extreme potential outcomes, when in reality, the extremes happen less often. If you have difficulty identifying the most likely scenario, it may be helpful to find a scenario that has some degree of negative outcome paired with some degree of positive outcome. For instance, “I’ll give the speech, and there will probably be some people who are bored and some people who are really interested.”
3. How many times have you made this prediction, and it came true? Another way to consider the usefulness of your worry is actually to count how many times the worst-case scenario has happened. If you’ve driven on the freeway 100 times in the past year and have never gotten into an accident, those odds indicate your worry may be disproportionate. Even if you have been in an accident, your level of worry may have made it feel like it was a 50% chance, thus causing unnecessary fear.
4. If the worst-case were to happen, what would you do to cope with it? People generally end their worrisome predictions right at the worst moment. You may find it helpful to think about what would happen next, specifically, what you would do to get through the difficult situation. If you do fail the test, you might be disappointed for the rest of the day, curl up on the couch with a pint of ice cream and watch T.V. Then you’ll probably get back on the horse by finding out what you did wrong and altering your study strategy so you pass the next time. Although failing an important exam is unpleasant, you probably have a lot you could do to deal with it effectively. Consider that, too!
5. What are the costs and benefits of worrying about this? Finally, examine how effective it is to worry about this situation. Some degree of worry may be helpful in motivating you to prepare. Too much, on the other hand, may paralyze you and become a self-fulfilling prophecy. And some things, no matter how much you worry about them, you don’t have any control over. In these latter two instances, the worry is self-defeating. It is unproductive worry.
When you identify a worry as unproductive, you can tell yourself, “Thinking about this is of no use to me now. Let it go.” Then, immediately refocus your mind on what’s actually going on around you. By rehearsing this behavior, intentionally letting go of worries again and again, you learn to become less consumed by anxiety and worry.
This technique comes from a cognitive behavioral therapy protocol for generalized anxiety. CBT for generalized anxiety has been found to be 70%-80% effective in significantly reducing anxiety symptoms, as compared to a 30% effectiveness rate of traditional talk therapy (Durham, 1995). CBT for anxiety works best with the help of a trained cognitive-behavioral therapist. If you or someone you know has problems managing anxiety, click here for more information about CBT for Anxiety.
Cognitive Behavioral Therapy Los Angeles is a therapy practice of expert psychologists with the highest level of training and experience in providing evidence-based treatment. Click the button below to ask a question or schedule a consultation to determine whether CBT is right for you.
Durham, R.C. (1995). Comparing treatments for generalized anxiety disorder: Reply. British Journal of Psychiatry, 166, 266-267.